Dr. Mekeme Mekeme Junior Barthelemy,
Central Hospital of Yaounde, Urology Department,
E-mail: juniormekeme@yahoo.fr,
Tel: (237) 677 67 62 40
© 2019 Sift Desk Journals. All Rights Reserved
VOLUME: 4 ISSUE: 1
Page No: 168-173
Dr. Mekeme Mekeme Junior Barthelemy,
Central Hospital of Yaounde, Urology Department,
E-mail: juniormekeme@yahoo.fr,
Tel: (237) 677 67 62 40
Mekeme Mekeme J.B 1,5, Fouda J.C.1,5, Mbede M.1,5, Mbassi A.1, Moby H.2 , Biyouma Marcella5, Fouda P.J.1,5,Angwafo Fru III5, Ngo Nonga B.5, Sosso M. A.5.
1. Urology Department, Central Hospital of Yaounde, Yaounde, Cameroon
2. Douala Laquintinie Hospital, Douala, Cameroon
3. Department of Surgery, General Hospital, Yaounde, Cameroon
4. University Teaching Hospital, Yaounde, Cameroon
5. Faculty of Medicine and Biomedical Sciences, University of Yaoundé I, Yaounde, Cameroon
Mekeme mekeme Junior Barthélémy, A RARE CASE OF EPIDERMOID CARCINOMA OF THE PENIS COEXISTING WITH BENIGN PROSTATIC ENLARGEMENT(2021)Journal of Anesthesia & Surgery 4(1)
Background
Penile cancers are rare tumours especially in circumcised male. Only few cases have been reported in Cameroon. Here, we describe the case of a patient with a penile epidermoid carcinoma associated with benign prostatic enlargement presenting as an ulcerated lesion at 2cm below the coronal sulcus and lower urinary tract symptoms.
Case presentation
A 77-year-old Cameroonian male presenting with an ulcero-necrotic circumferential tender lesion on the penile shaft associated with predominantly voiding lower urinary tract symptoms was admitted in our unit. The diagnosis of penile cancer and benign prostatic enlargement were confirmed following a needle biopsy of the lesion (Mucoepidermoid carcinoma of the penis pT3N3Mx grade I) and prostatic ultrasound (BPE grade III) respectively. A total penectomy and suprapubic simple prostatectomy by transvesical technique were performed.
Conclusions
Penile ulcerated lesions should always be surgically explored as wide excision and postoperative histological examination remain the only means of obtaining a precise disease definition and, consequently, administering the appropriate treatment.
Penile cancer is a rare cancer worldwide, constituting 1% of male cancers and the most common histological type is squamous cell carcinoma [1,2]. The incidence in Cameroon is 3% and only one case has been reported [3,4]. Squamous cell carcinoma (SCC) accounts for 95% of the histological types of penile cancer [5], but other rarer types, such as epidermoid carcinoma (EC), may also affect the penis. The origin of SCC of the penis is usually the squamous epithelial surface, while the Mucoepidermoid Carcinoma of the penis does not have a known source. EC can present as a papillary, exophytic plaque or ulcerated lesion. Although non-SCC types are not classified by risk, their behaviour and prognosis can be ascertained. Inguinal nodes followed by iliac nodes are commonly involved.
Benign prostatic hyperplasia (BPH), also known as benign prostatic hypertrophy, is a histologic diagnosis characterized by proliferation of the cellular elements of the prostate. Usually develops in middle-aged men and prevalence increase with age. BPH concerns the stromal and epithelial elements of the prostate arising in the periurethral and transition zones of the gland. The hyperplasia presumptively leads to enlargement of the prostate that perhaps reduce the bladder urine outflow. The aetiology is multi-factorial with age, hormones such as serum testosterone levels slowly but significantly decrease with advancing age. However, levels of oestrogenic steroids are not decreased equally. According to this theory, the prostate enlarges because of increased oestrogenic effects. Advanced age, obesity, increased fat intake, decreased physical activity, and diabetes increase the risk of BPH development [6]. BPH symptoms can be attributed to or are clinical manifestations of an increased prostate volume which is characterized by Lower urinary tract syndrome (LUTS), Bladder Outlet Obstruction (BOO), incomplete bladder emptying, acute and chronic urinary retention, UTI, urosepsis, bladder stones and haematuria. BPH diagnosis is based on the triad: digital rectal examination (DRE), Serum prostate-specific antigen (PSA) and endorectal ultrasound examination confirmed by an anatomopathological analysis of the surgical specimen after surgery. Urinalysis is the only laboratory test universally recommended for BPH.
To our knowledge a synchronous epidermoid penile carcinoma and benign prostatic hyperplasia have never been reported in a patient.
CASE REPORT
In January 2010, a 77-year-old male polygamous driver from Kribi District Cameroon consulted us for a 3 years history of difficulty in passing urine that progressed to complete failure to void necessitating placement of an indwelling catheter for acute urinary retention. The hospitalisation course was marked by discharge and follow-up as an outpatient while waiting for surgery indicated for a BPE. Due to financial constraints, patient was lost to follow up and presented to the surgical emergency unit of theYaoundé Central Hospital with a spontaneous gradually increasing painful circumferential ulcerated lesion on the penile shaft of 2 years duration associated with dysuria, urinary frequency, urgency, hesitancy, weak stream, incomplete emptying and generalised fatigue. He reported that the ulceration began spontaneously on the dorsal aspect of the glans in the perimeatal region around the indwelling catheter and increased in size over time to include the penile shaft. This was associated with agonizing pain, sleeplessness, itches and foul-smelling discharge. He first resorted to traditional remedies with potions and local dressing to no avail followed by self-ablation of the indwelling catheter. His past history is remarkable for circumcision and left herniorrhaphy at 11 and 15years of age respectively. He had no history of smoking, systemic diseases, phimosis, balanoposthitis, or condilomatosis.
On physical examination, the lesion was single, circumferential with an ulcero-necrotic infiltrative surface, poorly defined borders which bled easily to contact, tender, occupying the entire glans and extending about 2 cm below the coronal sulcus with an induration of the corpus cavernosum (Figures 1 and 2), and only 6 cm of healthy skin left on the distal penis. There were palpable inguinal nodes, three on the left and two on the right which were non tender, firm and fixed (Figure 3). The digital rectal examination revealed clean anal margin, normal anal tone, an enlarged firm, smooth, non tender, rubbery prostate with absence of the median sulcus.

Figure 1: dorsal surface of penis, ulcero-necrotic lesions

Figure 2: ventral surface of penis: ulcer-necrotic lesion

Figure 3: left inguinal lymph node shown by the arrow
Laboratory workup showed a total PSA of 0,94 ng/ml, serum calcium of 75,48mg/l, neutrophil predominant leucocytosis, normal urinalysis and negative HIV serology.
Biopsies of the penile lesion and bilateral inguinal lymph nodes were taken and revealed grade I invasive well differentiated penile epidermoid carcinoma. The ultrasound scan showed an enlarged prostate of 77ml, which was heteronodular with a protruding median lobe of 38g and a post residual volume of 158ml. Both kidneys were reported as normal with no hydronephrosis or stone.
A computed tomography (CT) scan of the thorax, abdomen and pelvis revealed multiple bilateral inguinal lymphadenopathy (Figures 4 and 5).
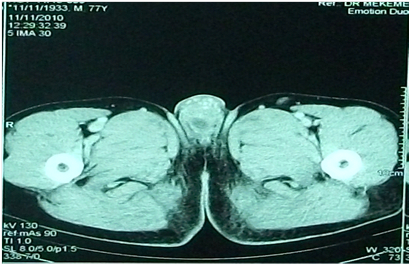
Figure 4: bulbar hyperdensity pelvic CT shown by the arrow.
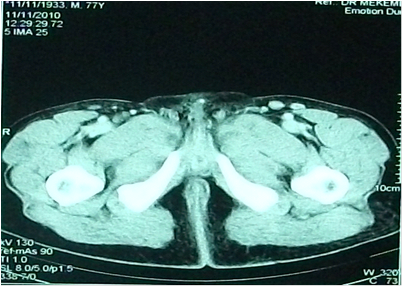
Figure 5: arrow showing enlarged inguinal lymph nodes on pelvic CT.
A suprapubic cystostomy was performed to dry out the urethra and relieve the patient's urinary symptoms. Daily local care and 6 weeks of quinolone antibiotic therapy were administered to the patient without significant improvement of the swollen inguinal lymph nodes or locoregional involvement.
The diagnosis of Epidermoid carcinoma of the penis pT3N3Mx grade I associated with stage III BPH was made.
The patient subsequently underwent a perineal urethrostomy, total penectomy with bilateral inguinal and pelvic lymphadenectomy and a suprapubic transvesical prostatectomy respecting the norms of carcinogenic surgery following a good multidisciplinary team meeting preparation including urologist, general surgeon, anaesthesiologist, psychologist and oncologist. An informed consent was obtained prior to the procedure.
The postoperative course was uneventful and our patient catheter was removed on postoperative day 21.
He was subsequently started on 5FU-CDDP and adjuvant radiotherapy. Every chemotherapy session was followed by a sequence of radiotherapy delivering 20GY of cobalt photons, 60 GY on the surgically excised margins. This therapy was marked by grade I radio-epithelitis and pollakiuria, which resolved after symptomatic treatment. By the second month postoperatively, all initially infiltrated tissues in the pubis and perineum were no longer visible. (figure 6)

Figure 6. Appearance on postoperative day 21 after removal of urinary catheter and perineal urethrostomy.
Penile cancer is relatively rare representing a serious health concern in different regions worldwide. Most penile cancers are squamous cell or epidermoid carcinomas of the glans or prepuce [7].
Penile cancer is most commonly diagnosed in men aged 50–70 years [8], our patient was about 75 years at the time of onset. Risk factors associated with penile carcinoma include age, poor socioeconomic status, smoking, multiple sexual partners, lack of personal hygiene, human papilloma virus, specifically subtypes 16 and 18, chronic balanitis and inflammation, phimosis, and redundant prepuce [4,9]. From our patient’s history we identified age, multiple sex partners, lack of personal hygiene and poor socioeconomic status as risk factors. Circumcision carried out early in the patient’s childhood is considered a protective factor.
As in our patient, patients with penile cancer often complaints of pruritus, pain, bleeding and foul-smelling discharge. The lesion can be in the form of a lump or nodule (47%), an ulcer (35%), or erythema (17%) [10].
Majority of patients present with a localized penile lesion, and physical examination defines tumour morphology, ulcerative or infiltrative characteristics, quality of surrounding tissues and assessment of urethral involvement, corpus cavernous and neighbouring structures.
Ultrasound or MRI may be useful in men with large tumours to evaluate the anatomical relationship with the surrounding structures. The diagnosis of epidermoid penile carcinoma is based on histopathologic studies from biopsy sample of the lesion. The biopsy is performed under local anaesthesia through deep core sampling. This will enable us determine the tumour histologic type, grade, classification, vascular and lymphatic involvement. Till date, 23% of those with normal inguinal regions have lymph node involvement.
Either CT or MRI can be used for lymph node staging based on size and shape criteria. However, MRI allows assessing functional aspects of lymph nodes.
Once there is histological evidence of the tumour, a thoraco-abdomino-pelvic CT scan appears to be the examination of choice for the detection of lymph node invasion [11]. For our patient, a thoraco-abdomino-pelvic CT scan highlighted multiple bilateral inguinal lymphadenopathy with no other anomalies suggesting secondary localization. Bone scintigraphy is indicated if there is evidence of bone involvement or hypercalcemia.
Localised disease can be managed by surgical excision (partial or total penectomy) or penis-preserving surgery (excisional biopsy and radiotherapy). In partial penectomy the recommended safety margin should be between 5 and 10 mm (but 15 mm in the case of G3 stage tumours) above the tumour for oncologic control [12] in order to enable the patient to urinate while standing. Therefore, the remaining penile length after partial penectomy must be at least 3cm, otherwise a total penectomy or emasculation with a perineal urethrostomy is recommended. Prophylactic localized inguinal lymphadenectomy may improve survival.
In advanced cases, surgery with or without radiation is often used for palliation or local disease control. Metastases may involve distant lymph nodes, lung, liver, brain, bone and is managed with chemotherapy.
Radiotherapy and chemotherapy are recommended as adjuvants because of their impact on patient preoperative general state and local adverse effects such as phlycten and difficult postoperative healing [12].
In this case report, antibiotics were administered to the patient without significant improvement of the inguinal lymphadenopathy or locoregional involvement. Following core biopsy result our patient’s tumour was classified as a grade I stage T3N3Mx. For oncologic control with respect to the tumour staging and grading, he underwent an emasculation, a perineal urethrostomy and bilateral inguinal and pelvic lymphadenectomy with quite satisfying results (figure 6). He had received three cycles of adjuvant chemotherapy and radiotherapy.
Surgical management is indicated in BPH when patients have complications such as acute urinary retention, recurrent gross haematuria, recurrent urinary tract infections, renal insufficiency, and bladder stones all due to prostatic obstruction, or lower urinary tract symptoms which are not responsive to medical treatment. Several surgical options exist for BPH depending on the prostate size such as endoscopy for small and medium-sized prostates or open prostatectomy for large prostate especially for those with coexisting problems such as bladder stones or other pathologies necessitating a surgical procedure.
Our patient had an epidermoid penile carcinoma stage T3N3Mx, which is the second penile carcinoma case to be reported in Cameroon and the only epidermoid one. Epidermoid carcinomas are rare as well as their description in the literature and this case report emphasizes on the importance of biopsy for an accurate and prompt management of any suspected penile lesion. Our case, should serves as an alert, enhancing the importance to conduct sensitizing campaigns on penile cancer in low-middle income countries especially those with limited resources.
The authors would like to thank all the clinicians and staff of the Central Hospital of Yaounde for the care of the patient
Statement of ethics
The authors have no ethical conflics to disclose, written informed consent was obtained from the patient for publication of this case report and any accompanying images.
A copy of written consent is avalable for review by the editor-in-Chief of the journal.
Any identifying material has been removed, including the patient’s name, date of entry, face or any distinctive features on the pictures taken
Disclosure statement
The authors have no conflicts of interest to declare
Funding
The authors received no financial support for the research, authorship, and /or publication of this article
Author’s contributions
-Mekeme contributed in the design of the study and writing of the manuscript
-Fouda contributed in critical reading
-Mbede collected the picture, and obtained the patient’s consent
-Mbassi contributed in critical reading
-Biyouma contributed to translate the French version to English
-All authors have read and approved the final version of the manuscript
List of abbreviations
|
GY |
Gray |
|
FU-CDDP |
Fluorouracil-Cisplastin induction Chemotherapy |
|
MRI |
Magnetic Resonance Imaging |
|
CT |
Computed Tomography |
|
PSA |
Prostate Specific Antigen |
|
HIV |
Human Immuno-deficiency Virus |
|
BPE |
Benign Prostatic Enlargement |
|
SCC |
Squamous Cell Carcinoma |
|
EC |
Epidermoid Carcinoma |
|
BPH |
Benign Prostatic Hyperplasia |
|
LUTS |
Lower Urinary Tract Symptoms |
|
MC |
Mucoepidermoid Carcinoma |
|
BOO |
Bladder Outlet Obstruction |
|
UTI |
Urinary Tract Infection |
|
DRE |
Digital Rectal Exam |
J E Heinlen, D D Buethe, D J Culkin (2012) Advanced penile Cancer. International Urology and Nephrology 44(1): 139-148. PMid:21814740
View Article PubMed/NCBIBarski D, Georgas E, Gerullis H, Ecke T (2014) Metastatic penile carcinoma - an update on the current diagnosis and Treatment options. Cent European J Urol 67(2): 126-132. PMid:25140224
View Article PubMed/NCBIDjeumi T, Guifo M.L, Mbassi A. Operations for Urologic Malignant Tumors or Suspected Neoplasms in a Resource-Limited Setting: Last Decade Experience in Cameroon. Cancer Sci Res. 2019; 2(2); 1-3.
View ArticleSando Z, Noubom M, Fouogue JT, et al. Penile carcinoma in medical poor settings in Cameroon: a case report. Adv Cytol Pathol. 2018;3(3):65-66
View ArticleFroehner M, Schöbl R, Wirth MP. Mucoepidermoid penile carcinoma: clinical, histologic, and immunohistochemical characterization of an uncommon neoplasm. Urology 2000 Jul 1; 56(1):154. 00530-6
View ArticleTeillac P. Prostatic Enlargement; Benign Prostatic Hyperplasia, National kidney and Urologic diseases information, clearing house 2006, US Department of Health and Human Service. 7
Shrikhande, S.S., Sirsat, M.V.: Muco-epidermoid carcinoma of the penis: re-ort of an unusual case. Brit. J. Urol. 46, 233-235 (1974) PMid:4823897
View Article PubMed/NCBIMaiche AG. Epidemiological aspects of cancer of the penis in Finland. Eur J Cancer Prev. 1992;1(2):153?158. PMid:1463977
View Article PubMed/NCBIMaden CJ, Sherman KJ, Beckmann AM et al (1993) History of circumcision, medical conditions and sexual activity and risk of penile cancer. J Natl Cancer Inst 85:19-24. PMid:8380060
View Article PubMed/NCBIHuben R, Sufrin G. (1991) Benign and malignant lesions of the penis. Adult and Pediatric Urology p. 1643
LONT AP, BESNARD APE, GALLEE MPW, VAN TINTEREN H, HORENBLAS H: A comparison of physical examination and imaging in determining the extent of primary penile carcinoma. BJU Int. 2003; 91: 493-495. PMid:12656901
View Article PubMed/NCBIAGRAWAL A, PAI D, ANANTHAKRISHNAN N, SMILE SR, RATNAKAR C. The histological extent of the local spread of carcinoma of the penis and its therapeutic implications. BJU Int 2000; 85:299-301 PMid:10671885
View Article PubMed/NCBI